|
||||||||||
Date: November 26, 2026
by Chaya Venkat
Viruses, like all pathogens, can be harmful in themselves. But there is a family of common viruses that is of particular significance to CLL patients because of the sometimes deadly interplay between the virus and the cancer. You will be in a better position to understand the risks from infections and from CLL therapy if you know what you are dealing with.
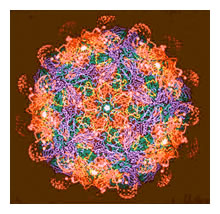
Meet the Family, the Herpes Family
Herpes is a family of many different viruses, literally dozens of them, but only 9 of them are of importance in humans.
Perhaps the most widely known members are Herpes Simplex types 1 and 2, the causes of oral and genital herpes. These are pretty serious conditions, especially in immune compromised patients. The others in the family may be even more important (and life-theratening) to CLL patients. They are identified as follows: Epstein-Barr virus (EBV), which causes infectious mononucleosis; Cytomegalovirus (CMV) which infects between 50% and 85% of adults in the United States by 40 years of age, and Varicella Zoster virus (VZV) which causes chicken pox — as well as shingles. The other herpes viruses in the "gang of nine" each cause its own set of signs and symptoms, different from the signs and symptoms of infection caused by the unfortunately familiar Herpes Simplex viruses.
Most Americans have herpes, either as genital herpes (GH), or as oral herpes ("cold sores"). The difference between "genital" Herpes and "oral" Herpes is in location only, not viral type. Many people mistakenly refer to HSV-2 as "genital herpes," and HSV-1 as "oral herpes," when in fact, Herpes types 1 and 2 can and do infect either area.
Experts estimate about 60 million Americans have the herpes virus that causes the genital form of herpes, with up to 500,000 new cases diagnosed each year. Herpes can be carried in saliva from contact with an open sore, and can be passed via incidental transmission from fingers or hand when the virus is active. Touching a sore and then touching another part of the body, or another person's body, can transmit the virus. Washing one's hands thoroughly with soap and water is the simplest way to inactivate Herpes virus that may be on skin.
Primary infection occurs through a break in the mucus membranes of the mouth or throat, via the eye or genitals or via minor abrasions or cuts in the skin. Because the virus is so widely distributed, most individuals are infected by 1-2 years of age. There are generally very few symptoms with the initial infection, excepting for minor sores at the location of the infection.
Once an individual is infected, however, the virus multiplies readily and becomes established as a systemic infection. During this period of primary infection, the virus enters peripheral sensory nerves and migrates along axons to sensory nerve ganglia in the central nervous system, CNS. Since the CNS is a so-called privileged site, out of bounds to much of the body's immune system, living quietly within this region allows virus to escape immune response. Except for periods of reactivation of the latent virus leading to recurrent disease, the virus maintains a life-long latent infection. During this latent infection of nerve cells, viral DNA is maintained as an episome (not integrated) with limited expression of specific virus genes required for the maintenance of latency — true latency. The delicate balance of latency may be upset by various disturbances, physical (injury, U.V, hormones, etc.) or psychological (stress, emotional upset — perhaps affecting immune system/hormonal balance). When a reactivation episode is triggered, the virus travels back down sensory nerves to body surfaces and replicates, causing tissue damage.
Carriers of HSV who are prone to cuts on fingers are susceptible to Herpes Whitlow, or Herpes infection of the fingers. Anyone with oral cold sores or genital outbreaks should avoid touching active Herpes lesions, wash theri hands right away in the event of contact and refrain from biting their nails for this reason. A Herpes infection in the eyes can lead to severe complications, including blindness, so extreme care should be taken to avoid transmission or transferal of the virus to the eyes.
Below is an excellent website that has a lot of easy to understand information about Herpes virus. I have pulled this quote from the site, just to make sure you understand the relevance of this topic to us.
"For women and men both, it's important to be aware that HERPES is more likely to reactivate when the immune system is not functioning well. Therefore, any illness or medical treatment that suppresses immune function may bring about a dramatic change in the frequency or severity of herpes outbreaks. People undergoing chemotherapy, for example, are likely to suffer from painful or lengthy recurrences and may require special medical care, including more aggressive antiviral therapy for HERPES".
http://www.herpesdiagnosis.com/complications.html
One quick point I would like to make. Much of the information I find relating to viral infections of various kinds, and how they effect immune compromised people, is from sites dealing with AIDS. Don't freak out, but there are a lot of similarities between acquired immune deficiency which is AIDS, and congenital immune deficiency which is one of the issues we deal with as leukemia patients, cancer-derived immune deficiency or iatrogenic immune deficiency due to use of chemotherapy drugs. In the case of AIDS, the immune function cells are compromised because of the HIV viral infection. With us CLL folks the immune deficiency is due to an unfortunate mutation(s) of some sort in our b-cells, and also due to the very drugs we have to take sometimes to control the disease. Both in CLL and AIDS, less than efficient immune function means we have to be more aware of opportunistic infections, latent infections reactivating more frequently and the greater virulence and severity of such infections.
It just so happens that the AIDS community is a lot more organized and proactive in their efforts to educate their people. I am just piggy backing and picking up what information I can, that is of direct use to us. There is no stigma here, a staggering majority of Americans are Herpes positive, we are all people struggling to find answers to complex questions.
If you click on the website URL above, scroll down to the picture of a person's thumb infected with Herpes Whitlow. This sort of an auto-inoculation, caused by, say, biting your finger nail when you have a herpes mouth sore, happens quite readily, especially in immune compromised people. How many of you macho guys out there look at this thumb and dismiss it as rough skin, perhaps because you have been doing "manly chores" round the house and you won't be caught dead using sissy moisturizing lotions? Well, left untreated, this viral infection can become quite a little problem, and more important, it can "drive the bus" as described below, rapidly increasing your WBC counts.
Stay healthy, people. Take care of yourselves. I am constantly amazed how much it helps to be pro-active in understanding the issues and making sure we get adequate healthcare. Our doctors and healthcare providers are dedicated, and hardworking. But they **are** overworked, and it is up to us to make sure we bring our concerns and symptoms to their attention. After all, who has more at stake in this dialogue?
VZV causes chicken pox and also shingles. Infection normally occurs in childhood and more than 90% of the world's children are known to be infected. Infection happens via respiratory tract or conjunctiva. After multiplication at the inoculation sites, virus spreads to bloodstream and reticuloendothelial system. Secondary multiplication involves skin and mucus linings, producing multiple sores filled with pus containing very high levels of infectious virus. Complications are rare, but may include infection of the central nervous system (CNS). After primary infection, the virus persists in sensory ganglia of CNS. It is not clear if this is a latent or a persistent infection but 'reactivation' after many years leads to a painful condition called "shingles" and can cause tissue damage. Shingles are most serious when cranial nerves are involved, affecting the face and head and in some situations it can lead to blindness.
The good news is that shingles can be treated with several anti-viral drugs available today. It is important that the anti-viral medications be started right away: the sooner you start, the quicker the symptoms can be controlled and the damage minimized.
CMV is the largest of the Herpes viruses, with a genome in the 240kbp range. CMV infection are slow to develop, taking anywhere from 7-14 days compared to less than 2 days for Herpes Simplex Virus. The cytomegalovirus has been studied extensively and its complete nucleotide sequence is known. CMV infection is common; 60% of the adult population have experienced infection by the age of 40. Most infections are asymptomatic. But in spite of the widespread distribution, CMV-related illness is rare and active (as opposed to latent) CMV infection only occurs in people with immune defects, specifically T-cell defects, such as CLL patients treated with chemotherapy drugs that are immune suppressive, bone marrow and solid organ transplant patients, whose immune systems must be suppressed in order for the graft to take, and AIDS patients. Transmission is believed to be by oral/respiratory route.
CLL patients will hear a lot about this member of the Herpes family. It is important and sometimes quite deadly principally because of the complications it induces in immune suppressed people. For that reason we will talk quite a lot about this member of the Herpes family.
Below is an abstract that talks about a small set of patients who underwent fludarabine treatment, for B-cell cancers of one sort or another. Months after therapy was completed, they developed new B-cell lymphomas, driven by the EB virus that used this window of opportunity to proliferate unchecked, because the individuals' immune system was depressed by the preceding chemo. Since EBV likes B-cells as its preferred residence and is able to confer some level of protection from cell death for the cells it does infect, you have all the makings of a new B-cell cancer.
The interesting thing here is that the new B-cell malignancy was a new cancer, not just an extension or re-emergence of the prior cancer. In a couple of cases it regressed on its own and in one case it responded to anti-viral therapy targeted at the EBV rather than the new cancer.
My thought is this: how many of our local oncologists are aware of this little twist? How many would just assume that it is simply the old cancer reappearing, that the therapy did not work, and they had better bring out even bigger guns to nuke the cancer? And all the time it could be due to an entirely different reason, such as an EBV (or CMV or some other virus) driven disease, and may require different therapy options, not make matters worse by further suppressing the immune system of the patient, giving the virus a better chance of proliferating.
Moral of the story, if there is one, is that if you relapse after chemotherapy, it might be smart to check out if EBV has suddenly decided not to be dormant and raise its ugly head. Does this suggest that people who go on fludarabine should also simultaneously also be on anti-virals, just as a precaution? I do not know the answer. But it may be worth checking out. Heck, the oncologists now know not to infuse Campath without simultaneously injecting all sorts of drugs to prevent opportunistic infections. Why is this not routine practice with all immunosuppressive chemotherapy drugs?
Source: Am J Surg Pathol; 26(5):630-6 2026 UI: 11979093
Epstein-Barr virus-positive B-cell lymphoproliferative disorders arising in immunodeficient patients previously treated with fludarabine for low-grade B-cell neoplasms.
Author: Abruzzo LV, Rosales CM, Medeiros LJ, Vega F, Luthra R, Manning JT, Keating MJ, Jones D
We describe five patients with treated low-grade B-cell neoplasms who subsequently developed Epstein-Barr virus (EBV)-positive B-cell lymphoproliferative disorders (BLPDs). The low-grade B-cell neoplasms were B-cell chronic lymphocytic leukemia in four patients and splenic marginal zone lymphoma in one patient. All patients had received treatment with fludarabine for the low-grade B-cell neoplasm, and three had also received Campath-1H. The EBV-BLPDs arose 2-12 months after completion of fludarabine therapy and morphologically resembled the EBV-BLPDs that occur in the setting of iatrogenic immunodeficiency. Molecular genetic studies showed that these lesions were clonally distinct from the low-grade B-cell neoplasm in three of four cases assessed. Two patients did not receive therapy for the EBV-BLPD. The lesions regressed spontaneously in both patients but recurred in one. One patient underwent surgical excision and remains without evidence of the EBV-BLPD. One patient received aggressive multiagent chemotherapy with a complete response initially, but the EBV-BLPD recurred after 12 months. One patient received antiviral therapy and responded completely but died 2 months later of an opportunistic infection. We conclude that patients with low-grade B-cell neoplasms treated with fludarabine, possibly in combination with other immune suppressive agents, may subsequently develop EBV-BLPDs that morphologically resemble other iatrogenic immunodeficiency-associated BLPDs. Most are clonally distinct from the underlying low-grade B-cell neoplasm. A subset of these lesions may regress without systemic therapy.
Now you know this virus can pack a wallop for CLL patients who are going through immune suppresive therapy. For more on this scary story read our article dated July 5, 2026 — EBV: The Enemy Within.
Want to know about viruses? Here is a neat website that you might want to visit. It was designed for third year medical students at the University of Cape Town, but I found it very easy to navigate and written in simple English: Virology Lectures. You can look up EBV and CMV under Herpes viruses.
This section will give you a little detail pertaining to how a viral infection may impact immune compromised CLL patients.
Consider what may happen to an immune compromised person when he/she is challenged by an insidious virus such as the Epstein-Barr virus (EBV). To get some terminology under our belt, the immune suppression can be congenital (as in CLL), acquired (such as in AIDS), or iatrogenic (caused as a side effect by use of chemotherapy drugs).
As we have learned in previous articles, EBV is present as a latent virus in almost all of us, like all the other Herpes viruses we discussed. In a healthy individual, the virus stays dormant, and a stalemate exists between the immune system and the virus. Once infected, the virus is next to impossible to eradicate completely, but neither can it do much harm with an active immune surveillance in place.
Along comes our hapless CLL patient, with reduced and/or dysfunctional T-cells, reduced levels of gamma-globulins and other crucial assets of the immune system. The EBV virus may use this window of opportunity to come out of dormancy and reactivate, at a time when the defenses are down. Since its favorite home is B-cells, out go the chemical messages to the body to produce more B-cells. Obediently, the body produces more and more B-cells, and the vast majority of them are the CLL clonal B-cells, pretty useless in fighting the infection. This is a case of clonal proliferation of B- cells, directly caused by the EBV seizing its chance.
The sudden and rapid increase in WBC numbers will be alarming to most patients. Once the driving force behind the growth spurt is identified, be it EBV, CMV, Hepatitis C or what ever, it becomes more feasible to target ways of controlling its proliferation and therefore put brakes on the lymphoproliferation.
Couple of weeks ago I discussed on CLL Topics an article in the Journal of New England Medicine, in which 9 patients with Splenic Lymphoma ( a close cousin of CLL) who also happened to be infected with Hepatitis- C were treated with interferon alpha, which is an anti-viral drug. In the process of killing the Hepatitis-C viruses, apparently the interferon also killed all the infected B-cells, thereby putting the patients (8 out of 9) into complete remission! Talk about making lemonade when you have too many lemons! Once in a while you get to see this kind of serendipity that works in our favor.
Even in patients who do not have CLL, but who are immune compromised in some fashion, say as a result of immune suppressing drugs given in the course of a solid organ transplant or bone marrow transplant (the patient would reject the organ or bone marrow, and the transplant would be a failure, without these drugs), the EBV virus can cause a sudden explosion of lymphocytes. In this case, the lymphocytes created are not clonal, but polyclonal. Very often, this sort of a post transplant lympho proliferative disease ("PTLPD" don't you just love all these acronyms?) can be resolved by reducing the amount of immune suppression, by decreasing the amount of drugs administered. It is a fine line to walk, just enough drugs to keep the transplant from getting rejected, but not so much that there is risk of PTLPD.
The moral of my story is quite simple. If you have a relatively stable disease, it is bumping along at a fairly predictable rate, and you are happy to consider yourself one of the smoldering variety, and suddenly, out of the blue, for no reason that you can think of, the disease takes off on you, galloping at a fast clip, time to consider perhaps you have a viral driver of this particular bus. Besides accelerated proliferation of the WBC, viral interaction with the CLL cells can also give rise to some types of transformation to more aggressive forms, such as diffuse large cell, PLL, or Richter's transformation.
Things out of the ordinary start happening, think about potential infection of some sort, get yourself checked out. Sometimes, you have to be a little assertive in your healthcare requests, most local oncologists are resigned to accept proliferation as a part of life with cancer, and are unwilling to entertain ideas such as this. Who knows, you might just be lucky like those guys with splenic lymphoma, come away with a complete remission as a result of relatively simple anti-viral therapy.
Below are three PubMed abstracts that you can read, to get more detail behind these concepts I have been discussing. My next article will discuss some of the newer antiviral drugs that are available to us. Come to think about it, besides the "home runs" of monoclonal antibody drugs like Rituxan and Campath, it is the little "bunts" consisting of better antibiotics, better antivirals, better ways around anemia, better diagnostics to figure out what is wrong in the first place, and so on, these may not seem such a big deal; but when you are looking at the big picture, but these little improvements add up to significantly better survival chances for all of us. Your best protection is awareness of the options available to you out there.
Anticancer Res 1989 Nov-Dec;9(6):1457-76
Persistent active herpes virus infection associated with atypical polyclonal lymphoproliferation (APL) and malignant lymphoma.
Krueger GR, Manak M, Bourgeois N, Ablashi DV, Salahuddin SZ, Josephs SS, Buchbinder A, Gallo RC, Berthold F, Tesch H.
Department of Pediatrics, University of Cologne, Germany.
This study focuses on lymphoproliferative diseases associated with persistent infection by Epstein-Barr virus (EBV) and human herpes virus 6 (HHV-6). A suggestive premalignant lymphoproliferative state is distinguished from malignant lymphoma and identified as "atypical polyclonal lymphoproliferation" (APL). Sixteen cases of herpes virus (HHV)-associated APL are compared with 21 cases of HHV-associated malignant lymphomas (ML), with 108 cases of EBV or HHV-6 related acute infections mononucleosis, with 14 cases of seronegative non- specific lymphoid hyperplasia and with 304 cases of HHV-unrelated ML. Six cases of APL and two ML occurred in AIDS patients, two cases in Sjogren's syndrome, one in a kidney allograft recipient, and the remaining cases had no identified underlying disease. APL was histologically reminiscient of excessive infectious mononucleosis, while other cases of Castleman's disease or even of malignant lymphoma. Seropositive APL and ML contained significantly more virus genome than is found in latent background infection. There was no histologic difference between HHV-6 or EBV-positive APL or ML, although both viruses infect different lymphocyte populations. From histology alone, seropositive ML cases were not distinguished from seronegative ones, yet persistent active EBV and HHV-6 appear to predominate in follicular center cell- and immunoblastic lymphoma and in HOdgkin's disease. Although no a direct oncogenic activity of these viruses could be observed in our cases, they may contribute to lymphomagenesis by inducing progressive lymphoproliferation.
PMID: 2560617
___________
Curr Opin Hematol 1999 Jan;6(1):25-9
Epstein-Barr virus and lymphoproliferative disease.
Mosier DE.
Department of Immunology-IMM7, The Scripps Research Institute, La Jolla, CA 92037
The Epstein-Barr virus is a ubiquitous human herpesvirus that is associated with an increasing number of human malignancies. Among these are Epstein-Barr virus-associated lymphoproliferative diseases in immunocompromised patients, a spectrum of mainly B-cell diseases that range from polyclonal lymphoproliferative diseases, which resolve when immunosuppression is halted, to highly malignant lymphomas. Progress has identified Epstein-Barr virus gene products involved in B-cell transformation, variation in Epstein-Barr virus transforming genes, distinct target cell populations with differing regulation of Epstein-Barr virus expression, and selective recruitment of other supportive cell types as factors in the heterogeneity of lymphoproliferative diseases. New therapeutic approaches to treat lymphoproliferative diseases are also being developed. Finally, xenotransplantation poses new risks for the introduction of Epstein-Barr virus-like viruses and more aggressive lymphoproliferative diseases in heavily immunosuppressed patients.
____________
Mod Pathol 1999 Feb;12(2):200-17
Immunodeficiency-associated lymphoproliferative disorders.
Knowles DM.
Department of Pathology, Cornell University Medical College, New York, NY
The incidence of lymphoproliferative disease is significantly higher in individuals who have congenital, acquired, or iatrogenically induced immunodeficiency. The immunodeficiency-associated lymphoproliferative disorders are clinically and pathologically heterogeneous, are of variable clonal composition, and vary according to the immunodeficiency syndrome. Nonetheless, they share several features, including frequent origination in or involvement of extranodal sites, diffuse aggressive histology, B-cell lineage derivation, association with the Epstein-Barr virus (EBV), and, often, rapid clinical progression. Reactive and atypical lymphoid hyperplasias and malignant lymphomas occur in association with congenital (primary) immunodeficiency. Post-transplantation lymphoproliferative disorders are often comprised of a polymorphic cell population, making it difficult to identify their benign or malignant nature by histopathologic criteria alone. Recent studies suggest that they are divisible into plasmacytic hyperplasias, polymorphic lymphoproliferative disorders, and malignant lymphomas. The plasmacytic hyperplasias are polyclonal and generally regress spontaneously following withdrawal of immunosuppression. The malignant lymphomas are monoclonal, possess a variety of genetic alterations, and generally progress despite aggressive therapy. The polymorphic lymphoproliferative disorders are also monoclonal but display variable clinical behavior, their progression apparently correlating with bcl-6 gene mutation. Non-Hodgkin's lymphoma (NHL) is the second most common AIDS-related neoplasm and an AIDS-defining illness. AIDS-related NHLs are divisible by anatomic site of origin into systemic (nodal/extra nodal), primary central nervous system, and body cavity-based (primary effusion) lymphomas; and by histopathology into Burkitt's and Burkitt's-like lymphoma, large cell lymphoma, and large cell immunoblastic (plasmacytoid) lymphoma More than 90% are monoclonal B-cell neoplasms. The primary effusion lymphomas contain the Kaposi's sarcoma-associated herpesvirus. Multiple molecular pathways appear to operate in AIDS lymphomagenesis and some may be preferentially associated with specific histopathologic categories or anatomic sites of origin. In conclusion, the immunodeficiency-associated lymphoproliferative disorders often represent a significant diagnostic problem requiring correlative analysis of the clinical behavior of the patient with the histopathology, immunophenotype, clonal composition, viral content, and genetic alterations of the lymphoproliferative disorder. They also represent an important biological model for studying the development and progression of lymphoid neoplasia.
PMID: 10071343
____________
The title of the paper cited below says it all: "Hostile takeovers: viral appropriation of the NF-kB pathway "
As far as I am concerned, this is a "must-read" paper. A little tough on the jargon, but it addresses two issues we have been discussing in recent weeks, namely influence of viruses on lympho-proliferation, and activation of the NF-kB pathway as a mechanism for giving cancer cells unfair advantages in survival and proliferation.
I thought this paper was so relevant that I took snippets from the introduction and reproduced them below. Also attached is a PubMed abstract that specifically talks of activation of the NF-kB pathway by Herpes Simplex Virus (HSV-1).
Hostile takeovers: viral appropriation of the NF-kB pathway
http://www.jci.org/cgi/content/full/107/2/143
The transcriptional regulator NF-kB that we have been discussing on this site controls the expression of well over 100 target genes, the majority of which participate in the host immune response. Because of this extensive role in immune action, NF-kB has been termed the central mediator of the immune response. There is little doubt that NF-kB participates at multiple steps during oncogenesis and the regulation of programmed cell death.
For several reasons, the NF-kB pathway provides an attractive target to viral pathogens. In this review, we will describe strategies that viruses have evolved to modulate the NF-kB pathway, to enhance viral replication, host cell survival, and evasion of immune responses. Activation of NF-kB constitutes an obvious target because many of its target genes — growth factors, cytokines and their receptors, and proto-oncogenes — profoundly influence the host cell cycle. In addition, some viruses exploit the antiapoptotic properties of NF-kB to evade the host defense mechanisms that limit replication by killing infected cells, or conversely to trigger apoptosis as a mechanism to increase virus spread.
Perhaps not surprisingly, the persistent activation of the NF-kB pathway maintained by certain viruses contributes to oncogenic transformation . There is evidence to demonstrate that NF-kB family members contribute to human oncogenesis. Localization of NF-kB– encoding genes at sites of chromosomal translocations and genomic rearrangements in cancer, high levels of NF-kB activity in many breast cancer cells, and constitutive nuclear NF-kB complexes in Hodgkin's lymphoma cells all support this view. Furthermore, as discussed below, viral oncogene products, including human T-cell leukemia virus type 1 (HTLV-1) Tax protein and Epstein-Barr virus latent infection membrane protein 1 (EBV LMP1), each act by unique mechanisms to disrupt NF-kB regulation and initiate viral transformation.
____________
J Biol Chem 2026 Aug 3;276(31):28759-66
Activation of I kappa b kinase by herpes simplex virus type 1. A novel target for anti-herpetic therapy.
Amici C, Belardo G, Rossi A, Santoro MG.
Department of Biology, University of Rome Tor Vergata, 00133 Rome, Italy.
Herpes simplex viruses (HSV) are ubiquitous pathogens causing a variety of diseases ranging from mild illness to severe life- threatening infections. HSV utilize cellular signaling pathways and transcription factors to promote their replication. Here we report that HSV type 1 (HSV-1) induces persistent activation of transcription factor NF-kappa B, a critical regulator of genes involved in inflammation, by activating the I kappa B kinase (IKK) in the early phase of infection. Activated NF-kappa B enhances HSV-1 gene expression. HSV-1-induced NF-kappa B activation is dependent on viral early protein synthesis and is not blocked by the anti-herpetic drug acyclovir. IKK inhibition by the anti-inflammatory cyclopentenone prostaglandin A(1) blocks HSV-1 gene expression and reduces virus yield by more than 3000-fold. The results identify IKK as a potential target for anti-herpetic drugs and suggest that cyclopentenone prostaglandins or their derivatives could be used in the treatment of HSV infection.
PMID: 11387335
____________
Anti-inflammatory drugs such as NSAIDs can block the critical NF-kB pathway. Can this slow down cancer progression? The attached is an article from Reuters Health that is really worth reading.
One of the potential viral drivers of cancer growth, especially in lymphomas and leukemia was introduced above - CMV (Cytomegalovirus). It is present in the vast majority of adult humans. It stays in a dormant most of the time, except in situations where the immune system is not functioning right; as in CLL patients, right after heavy duty chemotherapy or bone marrow transplant, when the immune system is not up to the job of keeping the virus under check. Post transplant lymphoproliferative disease (PTLPD) is one of the most serious and potentially fatal complications of transplants, whether it be bone marrow, solid organ or stem cells, and CMV is one of the most common viral drivers of this disease.
I knew all about aspirin as an anti-inflammatory, a good blocker of NF-kB pathway, and an inhibitor of Cox-1 and Cox-2 enzymes. What came as a surprise is that it is also an excellent killer of viruses, including the dreaded CMV and Herpes virus.
Please be careful before you start self medication however. CLL patients with low platelets - and therefore in danger of bleeding problems and general thrombocytopenia - should be extremely careful about taking blood thinners; and aspirin is a blood thinner. But in the absence of contra-indications, if you are in early stages of W&W, you might want to talk to your doctor about the advisability of taking anti-inflammatory materials, whether they be "drugs" such as aspirin, Celebrex, etc., or food based supplements such as curcumin.
Proceedings of the National Academy of Sciences Early Edition 2026;10.1073/pnas052713799.
Anti-Inflammatory Pain Relievers May Fight Viruses
NEW YORK (Reuters Health) - Certain pain relievers, including aspirin, might actually be able to fight some viruses instead of just treating virus symptoms such as fever, researchers report. In a laboratory study, investigators in New Jersey have found that the group of pain relievers that inhibit an enzyme known as COX-2 prevent reproduction of a virus called human cytomegalovirus (CMV). This squelching effect, which can be accomplished by aspirin and other drugs, might very well apply to other viruses, according to an independent expert. Even if the results apply only to CMV, the findings will be important if they're confirmed by clinical studies. CMV infects most adults, without causing illness, but it can be deadly in people with weak immune systems, such as AIDS patients. Also, CMV infection in pregnant women is a leading cause of birth defects, especially hearing impairments. The effect of inhibition of COX-2 on CMV was first studied several years ago. A laboratory study showed that when muscle cells infected with CMV were treated with aspirin, the reproduction rate of the virus was cut in half. The current study confirmed this result. When Dr. Thomas E. Shenk of Princeton University and colleagues infected skin cells with CMV, they found that inhibiting COX-2 reduced the virus reproduction rate more than 100-fold. The researchers used three experimental compounds in the study that specifically inhibit COX-2 alone. They also used another drug that is known to inhibit both COX-2 and COX-1, another type of enzyme. Traditional drugs such as aspirin and ibuprofen inhibit both enzymes, but a newer class of drugs, known as COX-2 inhibitors, are more targeted. But the New Jersey team went further than the other researchers--they showed why inhibitors of COX-2 have this effect. They already knew that the drugs block the production of a naturally occurring chemical in the body called prostaglandin E2. This and other prostaglandins are responsible for the pain, fever and inflammation that develop in a wide range of disorders. Shenk and his associates added to this knowledge by showing that prostaglandin E2 is vital to the reproduction of CMV. They added prostaglandin E2 to CMV-infected cells in which virus reproduction had been blocked by an inhibitor of COX-2. Prostaglandin E2 restored virus reproduction, the researchers report in the Proceedings of the National Academy of Sciences Early Edition, released online February 26. There is evidence that prostaglandins play a role in the reproduction of other viruses, Dr. Edward Mocarski, Jr. of Stanford University suggests in a journal commentary. An example, he notes, is the herpes simplex virus. One strain of this virus causes cold sores and another causes genital herpes infections. If scientists confirm that prostaglandins are involved in herpes and other viral infections, drugs that suppress prostaglandins might be "an auxiliary means of controlling infection," according to Mocarski.
_____________
Now we know that viruses can take advantage of an immune-suppressed system and make a bad situation worse. But can they actually cause CLL (or other cancers)? This was the question from a friend. I thought I would share my response to her with the rest of you, since it is relevant to the discussion we have been having on the subject.
I do not have any information that says, unequivocally, that CLL is caused by viral infection. There is such evidence for other cancers, for example T-cell leukemia is caused by HTLV (human t-cell leukemia virus), Burkitt's lymphoma is caused by EBV and cervical cancer is caused by HPV. In fact, the latest issue of Journal of New England Medicine has a breakthrough report on a vaccine for cervical cancer, which is in reality a vaccine for HPV virus. No such direct causative link has been established between a specific virus and CLL. That may change in the future.
Having said that, there is little doubt that a large number of viruses take advantage of reduced immune function to invade and establish themselves. Some of these, like EBV, and a variety of Herpes viruses, are already present in a dormant state in most people, it is just a case of the virus seizing its chance to come out of hiding and proliferate. Many of these viruses are so-called DNA viruses and prefer B-cells as their hosts, hence the proliferation of these cells as the viral load goes up.
New information is coming to light on activation of the crucial NF- kB pathway by viral signals. The original event that created a genetically malformed CLL cell may not have been driven by a virus. But it sure sounds like they can be part of the reason why the cancer grows, rather than staying dormant and undetected.
The latest research says that an alarming percentage of "normal" people have detectable CLL clonal populations, detectable by careful flow cytometry. Majority of these people will never develop clinically significant CLL. These people are the ultimate "smolderers", and they may never know and never have to deal with CLL. Others, if they are unfortunate enough to have more weakened immune systems to begin with, and/or a happenstance viral infection of some sort to help them on their way, they may get to the point where CLL gets diagnosed and becomes an issue.
I am not sure there is anything we can do ahead of time to avoid this disease. But what we can do, after the fact so to speak, is to take viral infections seriously. Shingles and oral Herpes sores are not just painful nuisances, they can be the viral drivers that makes the CLL progress faster than otherwise, get you out of w&w or remission and back into therapy sooner than otherwise.
It is not always easy to identify viral infections, it requires careful testing and culturing to identify the specific virus. The other problem is that unlike broad spectrum antibiotics, which can deal with a host of bacterial infections, there are few anti-viral medications that can effectively handle a variety of viruses. In fact, till recently, there were few effective anti-virals. Some of that changed because of the intense research scrutiny on AIDS, another deadly disease caused by a virus. Interferon therapy is another approach to killing stubborn viruses like Hepatitis C virus. It is not something to be considered lightly, since interferon therapy has significant side effects, makes people sick while taking it.
Bottom line, treat each and every viral infection as a serious matter. Not all local GPs or general purpose oncologists are familiar with the link between viral infections and immune cell cancers like CLL, and they may not understand what the fuss is all about. This is where it helps if **you** are aware of the information, perhaps you can print out some of the papers and abstracts that we reference in this website. A well documented request will get you more attention than a garbled complaint
Does HPV cause cervical cancer?
That debate seems to be settled for HPV and cervical cancer. For details see: HPV FAQ. Here is a quote from that document:
"Does HPV cause cervical cancer? Yes, high-risk types of genital HPV are linked to cervical cancer. Most HPV infections go away by themselves and don't cause cancer. But high-risk HPV that does not go away over many years increases the risk of cervical cancer. Abnormal cells can develop when high-risk types of HPV don't go away. If these cell changes are not detected and treated and persist for many years, they can lead to cervical cancer."
There are a lot of pieces of the puzzle we do not have, yet. This much is clear: a subset of women with HPV are for some reason unable to deal with this infection and keep it in check. They are immune compromised in some fashion, for example because they have a disease like CLL, or AIDs, or have been through a heavy course of immune suppressing chemotherapy in the process of organ or bone marrow transplants, or chemotherapy for some other reason. In such cases, in a percentage of the women, the HPV will seize the window of opportunity to proliferate. We are back to the original question we discussed in many of my previous articles. The original mutation of a single cell that was the ground zero of the cancer may have not been caused by the virus. I say may not, because the jury is still out on that. But once the mutation exists, and you then throw into the brew HPV viral infection, coupled with an inefficient immune system that is not capable of dealing with the infection, and you have a scenario that may well lead to cervical cancer.
What makes the report in the New England Journal of Medicine (see abstract below) so interesting and encouraging is that in the process of vaccinating young women against HPV (which by itself is no small accomplishment, it has not been done before), in this well constructed and well documented study, they achieved 100% efficiency in preventing cervical cancer in the experimental group. Here is a case where controlling the viral driver of the disease prevented the disease grabbing a foothold in the first place, and certainly prevented any stray mutation from becoming cancerous.
I am sticking out my neck here, and please, bear in mind I too am just a lay-person and these are my personal opinions: I am coming to the conclusion that while CLL is initiated by a random act of genetic mutation, and allowed to develop into a small clonal population by an immune system sleeping on the job, in a significant percentage of patients the progression of the disease may be getting accelerated due to secondary viral infections. PTLPD (post transplant lymphoproliferative disease) is well documented: lymphomas that occur in people who have received immune suppressive drugs in the course of organ or bone marrow transplant. Well, if heavy duty immune suppression is the necessary condition for virally driven lymphomas, it seems logical to me that this is a mode of disease progression in CLL patients that should be of concern to us all. Heck, we **know** we are immune compromised! Is this the reason why there is so much variability in the way the disease behaves in different people? Can we keep more people in early stage w&w, in relative good health, by doing a better job of protecting them against viral infections? I realize, this is easier said than done, since it is not always possible to identify the nature of the viral infection, and we are woefully lacking in many broad spectrum antivirals.
Besides looking for broad spectrum antivirals, the other approach that is being explored is to improve the general immune competency of the patient, and this too is being investigated. Someday, we will know how to grow the patient's own healthy immune system cells into large armies in a laboratory, then inject them back to fight the good fight; no complications of host-versus-graft etc since we will be using the patient's own cells in the process. My hope is that CLL patients treated in this fashion early enough in their disease progression will never need therapy, never need to worry about all the other complications like AIHA and thrombocytopenia that raise their ugly heads as the CLL progresses. May be I am unduly optimistic, but I do believe the next generation of CLL patients, our sons and daughters who may acquire this disease as a "familial gift" from us, will be the ones to benefit fully from the breakthroughs happening now. Yes, I would like it to be sooner, so that my husband and all of you out there can also benefit. But as a devoted mother of a lovely daughter, I take comfort that if she ever faced this monster, she will have more help fighting it, and defeating it. So, keep participating in those clinical trials, just do it with your eyes wide open, and clear in your own head as to why you are doing it!
Controlled Trial of a Human Papillomavirus Type 16 Vaccine
Laura A. Koutsky, Ph.D., Kevin A. Ault, M.D., Cosette M. Wheeler, Ph.D., Darron R. Brown, M.D., Eliav Barr, M.D., Frances B. Alvarez, R.N., Lisa M. Chiacchierini, Ph.D., Kathrin U. Jansen, Ph.D., for the Proof of Principle Study Investigators
Volume 347:1645-1651, November 21, 2026, Number 21
BACKGROUND: Approximately 20 percent of adults become infected with human papillomavirus type 16 (HPV-16). Although most infections are benign, some progress to anogenital cancer. A vaccine that reduces the incidence of HPV-16 infection may provide important public health benefits.
METHODS: In this double-blind study, we randomly assigned 2392 young women (defined as females 16 to 23 years of age) to receive three doses of placebo or HPV-16 virus-like-particle vaccine (40 µg per dose), given at day 0, month 2, and month 6. Genital samples to test for HPV-16 DNA were obtained at enrollment, one month after the third vaccination, and every six months thereafter. Women were referred for colposcopy according to a protocol. Biopsy tissue was evaluated for cervical intraepithelial neoplasia and analyzed for HPV-16 DNA with use of the polymerase chain reaction. The primary end point was persistent HPV-16 infection, defined as the detection of HPV-16 DNA in samples obtained at two or more visits. The primary analysis was limited to women who were negative for HPV-16 DNA and HPV-16 antibodies at enrollment and HPV-16 DNA at month 7.
RESULTS: The women were followed for a median of 17.4 months after completing the vaccination regimen. The incidence of persistent HPV-16 infection was 3.8 per 100 woman-years at risk in the placebo group and 0 per 100 woman-years at risk in the vaccine group (100 percent efficacy; 95 percent confidence interval, 90 to 100; P<0.001). All nine cases of HPV-16-related cervical intraepithelial neoplasia occurred among the placebo recipients.
CONCLUSIONS: Administration of this HPV-16 vaccine reduced the incidence of both HPV-16 infection and HPV-16-related cervical intraepithelial neoplasia. Immunizing HPV-16-negative women may eventually reduce the incidence of cervical cancer.
__________
 Enter Keywords: |
———
Disclaimer: The content of this website is intended for information only and is NOT meant to be medical advice. Please be sure to consult and follow the advice of your doctors on all medical matters.
Copyright Notice:
Copyright © 2026-2007 CLL Topics, Inc. All Rights Reserved.
All materials contained on this site are protected by United States copyright law and may not be reproduced, distributed, transmitted, displayed, published or broadcast without the prior written permission of CLL Topics, Inc. You may not alter or remove any trademark, copyright or other notice from copies of the content.
However, you may download and print material from CLLTopics.org exclusively for your personal, noncommercial use.
———