|
||||||||||
Date: August 21, 2026
by Chaya Venkat
Index Page for Articles on
Best Practices

The CDC (the Centers for Disease Control) and infectious disease experts are desperately trying to get the word out: staph infections have jumped the antibiotic barrier and have now become “super bugs”.
 Why is this relevant to CLL patients? As usual, CLL — or treatment for CLL — leaves our patient group with various levels of immune deficiency. As a group we are more vulnerable than the general population to opportunistic infections. The more advanced the CLL and the more immune suppressive the therapies already used, the less is a patient able to mount an effective immune response to overcome infections. Drug resistant strains of staph pose a special hazard in these circumstances, since they do not respond to the usual first-line treatments. Awareness of the threat, a willingness to seek medical help quickly, accurate diagnoses and effective treatment are therefore critical. In addition there are things a CLL patient can do to improve his or her chances of not getting infected in the first place.
Why is this relevant to CLL patients? As usual, CLL — or treatment for CLL — leaves our patient group with various levels of immune deficiency. As a group we are more vulnerable than the general population to opportunistic infections. The more advanced the CLL and the more immune suppressive the therapies already used, the less is a patient able to mount an effective immune response to overcome infections. Drug resistant strains of staph pose a special hazard in these circumstances, since they do not respond to the usual first-line treatments. Awareness of the threat, a willingness to seek medical help quickly, accurate diagnoses and effective treatment are therefore critical. In addition there are things a CLL patient can do to improve his or her chances of not getting infected in the first place.
Staph (full scientific name Staphylococcus aureus, also called S. aureus) are common bacteria that colonize and live on the skin and in the nose of about a third of the general population. Staph germs can live like this for long periods without harming their host or causing symptoms. However, if there is a break in the patient’s skin due to injury or surgery, or if the person’s immune system is not working as well as it ought to, the staph colony can use the window of opportunity and cause infections. It is the quintessential “opportunistic infection”, waiting patiently for the window of vulnerability to strike its victim.
Staph frequently causes localized skin infections, such as infected hair follicles (“folliculitis”), boils (“furuncles”), and shallow, fluid-filled blisters surrounded by yellow crusts (“impetigo”). It can also cause external and internal abscesses and spread into the bones (osteomyelitis), lungs (staphylococcal pneumonia), blood (bacteremia or sepsis), damage to heart valves (endocarditis), as well as other organs. Staph is communicable infection in that it can be passed from both infected or merely colonized people (people who have staph germs on them, but no infection) to other people through skin contact or through contaminated objects, such as shared towels, personal grooming items.
 Used to be, Staph infections were acquired when patients were in a hospital or long-term care facility, where the germs have gradually evolved to become more resistant. Widespread use of antibiotics and the generally poor immune status of patient populations have led to the development of antibiotic-resistant strains of all sorts of bugs. In the good old days, penicillin was used to treat staph infections and it was more than enough to kill the little blighters dead. Not so anymore. Most of the strains of the bacteria are now resistant to penicillin. The standard antibiotics for staph infection in recent years have been methicillin and flucloxacillin, which must be given intravenously. However, some strains of staph are becoming resistant to these treatments, as well.
Used to be, Staph infections were acquired when patients were in a hospital or long-term care facility, where the germs have gradually evolved to become more resistant. Widespread use of antibiotics and the generally poor immune status of patient populations have led to the development of antibiotic-resistant strains of all sorts of bugs. In the good old days, penicillin was used to treat staph infections and it was more than enough to kill the little blighters dead. Not so anymore. Most of the strains of the bacteria are now resistant to penicillin. The standard antibiotics for staph infection in recent years have been methicillin and flucloxacillin, which must be given intravenously. However, some strains of staph are becoming resistant to these treatments, as well.
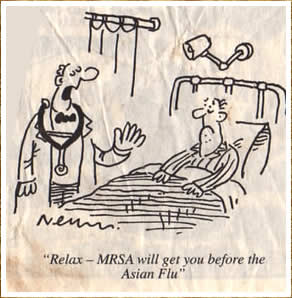
Risk factors increasing the likelihood of MRSA infection in the hospital include surgery, prior antibiotic therapy, admission to intensive care, exposure to a MRSA-colonized individual or health care worker, being in the hospital more than 48 hours, and having an indwelling catheter or other medical device that goes through the skin.
What makes the situation dangerous now is that resistant strains of staph are seen in unexpected places: in health clubs and gyms, day-care centers, grocery carts, playground equipment, door handles of public places. MRSA has now busted out of hospitals, and infectious disease experts are seeing a lot more of MRSA infections picked up in the general community. A growing number of MRSA outbreaks and deaths in settings such as prisons, day care facilities, military units, and competitive sports teams have doctors worried. These infections are occurring in people who do not have classic MRSA risk factors. A significant number of those affected have had to be hospitalized for what appears to be a simple but persistent skin infection or for a lung infection that is secondary to a case of influenza.
Here is an acronym you are going to see a lot more in the future: CA-MRSA (Community Acquired Methicillin Resistant Staphylococcus aureus). As immune compromised folks, watching out for MRSA is something that you cannot afford to ignore. Infections caused by MRSA are frequently resistant to a wide variety of antibiotics and are associated with significantly higher rates of morbidity and mortality, higher costs, and longer hospital stays than infections caused by non-MRSA microorganisms.
The hospital version of these resistant super bugs has long been known to doctors and is one of the main reasons why hospitals have increased the emphasis on infection control and hand-washing regimes in recent years. Thousands of cases of infections by resistant staph infections are reported annually, and some experts believe it to be one of the leading causes of hospital deaths. Staph infections take advantage of those with serious illnesses or compromised immune systems, easy victims ripe for the picking. But investigations have also revealed that the S. aureus strains involved in CA-MRSA are genetically distinct from those that have been causing hospital-acquired MRSA. The CA-MRSA are resistant to methicillin and other related antibiotics, such as oxacillin, dicloxacillin, or nafcillin, but frequently are not resistant to other types of antibiotics.
CA-MRSA is spread from infected or colonized patients to those around them through skin contact (such as sports- related cuts and abrasions), through droplets from the lungs or nose, or through exposure to contaminated objects, such as shared sports equipment, towels, eating utensils, toys, or playground equipment. This is a new phenomenon, and experts are calling it a “silent epidemic” that may get out of control if we do not pay attention to it. This once-rare drug-resistant germ now appears to cause more than half of all skin infections treated in U.S. emergency rooms, according to researchers who documented the superbug's startling spread in the general population. The two most virulent strains of community-acquired staph infections (strains known as US300 and US400) are also the two hardest to treat. It is time we learned a bit more about this deadly enemy.
Until recently, part of the problem with community-acquired MRSA (CA-MRSA) has been a lack of awareness in the medical community and the community at large. Historically, physicians have treated staph infections, based on their severity, with either over-the-counter triple-antibiotic ointments or with a standard course of antibiotics. They did not routinely order cultures to identify the organism and its antibiotic susceptibility profile unless the infection appeared extensive or the initial treatment was unsuccessful. With CA-MRSA, however, these conventional therapy options have frequently failed. A significant number of those affected have had to be hospitalized and a few previously healthy patients have even died.
Various staph super bugs are all around us – on skin, in the nose, on surfaces and in soil. "Wash your hands!" is the mantra preached by infection control instructors. Personal cleanliness and attention to details of hygiene are our single best defense. Officials with the federal Centers for Disease Control and Prevention estimate that drug-resistant staph infections may strike as many as 100,000 Americans each year, most of whom contract the infections in hospitals. In recent years, only the drug vancomycin has been widely successful at eradicating the infections, and researchers - fearing the bacteria will grow resistant to vancomycin as well - have been racing to find new alternatives.
If your doctor is “old school” and gives you a condescending pat on the head and tells you not to worry so much, I suggest you (1) bring him up to speed, or (2) get yourself a new doctor.
Type MRSA into any search engine on the Internet and you will see just how much of a furor there is on the subject. The trick is sorting out the credible information from the nonsense. Below are three good sources where you can get dependable information about MRSA.
CDC's MRSA Page
Living with MRSA - Community Health Bulletin
Physicians' Weekly Article on MRSA
 |
 |
 |
Published: Thursday, August 17, 2026
Associated Press
Staph infections are on increase
A once-rare drug-resistant germ now appears to cause more than half of all skin infections treated in U.S. emergency rooms, say researchers who documented the superbug's startling spread in the general population.
Many victims mistakenly thought they had spider bites that wouldn't heal, not drug-resistant staph bacteria. Only a decade ago, these germs were hardly ever seen outside of hospitals and nursing homes.
Doctors also were caught off-guard - most of them unwittingly prescribed medicines that do not work against the bacteria.
"It is time for physicians to realize just how prevalent this is," said Dr. Gregory Moran of Olive View-UCLA Medical Center, who led the study.
Another author, Dr. Rachel Gorwitz of the Centers for Disease Control and Prevention, said, "I think no one was aware of the extent of the problem."
Skin infections can be life-threatening if the bacteria get into the bloodstream. Drug-resistant strains can also cause a vicious type of pneumonia and even "flesh-eating" wounds.
The CDC paid for the study, published in today's New England Journal of Medicine. Several authors have consulted for companies that make antibiotics.
Researchers analyzed all skin infections among adults who went to hospital emergency rooms in 11 U.S. cities in August 2026. Of the 422 cases, 249, or 59 percent, were caused by methicillin-resistant Staphylococcus aureus, or MRSA. Such bacteria are impervious to the penicillin family of drugs long used for treatment.
The proportion of infections caused by MRSA ranged from 15 percent to as high as 74 percent in some hospitals.
"This completely matches what our experience at Vanderbilt Children's Hospital has been," said Dr. Buddy Creech, an infectious-disease specialist whose hospital was not included in the study. "Usually what we see is a mom or dad brings their child in with what they describe as a spider bite that's not getting better or a pimple that's not getting better," and it turns out to be MRSA.
 Enter Keywords: |
———
Disclaimer: The content of this website is intended for information only and is NOT meant to be medical advice. Please be sure to consult and follow the advice of your doctors on all medical matters.
Copyright Notice:
Copyright © 2026-2007 CLL Topics, Inc. All Rights Reserved.
All materials contained on this site are protected by United States copyright law and may not be reproduced, distributed, transmitted, displayed, published or broadcast without the prior written permission of CLL Topics, Inc. You may not alter or remove any trademark, copyright or other notice from copies of the content.
However, you may download and print material from CLLTopics.org exclusively for your personal, noncommercial use.
———