 |
||||||||||
Date: June 12, 2026
by Chaya Venkat
I read somewhere that the art of winning battles is to fight them one at a time and each one at the time and place of your choosing. If you are caught off-guard, off-balance, fighting on more than one front, without a battle plan clearly thought out and ready to kick into high gear at the right moment, your chances of winning are that much lower. There are no guarantees in life or battles and certainly no guarantees when it comes to cancer therapy. But the principle holds for fighting CLL as well. This article is all about the short term tactics used by Harvey (Harvey's Saga), our strictly hypothetical patient and my personal hero, as he tries to implement his long term strategy of dying of old age, some day in the distant future. Will he succeed in this goal? Only time will tell. There is a certain amount of luck involved and the best laid plans of mice and men often go awry. But I will give Harvey high marks for trying to fight the battle on his terms, in a manner of his choosing. Many of you have been following the saga of “Harvey” for several years now. Here is the latest chapter in that saga. It spells out Harvey’s long term strategy, his short term tactics, and what he is going to do next to try and reach his goal of dying of old age some day.
This is a quick re-cap of what has happened to our hypothetical hero thus far. Harvey was diagnosed with CLL in the summer of 2026. Actually, looking over his blood work from a year before that, it was clear he had had CLL since March 2026. Unfortunately, he also had poor risk cytogenetics, a complex karyotype that included double deletion of 13q and single deletion of 11q (ATM gene) by FISH testing (Cytogenetics of ATM and TP53; What Type of CLL Do You Have? FISHing for Answers). Patients with 11q deletion do not have good prognoses. Typically they progress rapidly, need therapy soon after diagnosis and tend to have bulky lymph nodes. For these residents of Bucket C, often there is none of the long term “Watch & Wait” that lets “smoldering CLL” patients go for years without needing much of anything by way of therapy. The classic research defining long-term prognosis for 11q (ATM) deleted patients was done by Dohner, Stilgenbauer, et al. If you have this cytogenetic abnormality, theirs is a “must read” article. The abstract is below and you can read the full text by simply clicking on the link.
Full-text Blood Journal Article
Blood. 1997 Apr 1;89(7):2516-22.
11q deletions identify a new subset of B-cell chronic lymphocytic leukemia characterized by extensive nodal involvement and inferior prognosis.
Döhner H, Stilgenbauer S, James MR, Benner A, Weilguni T, Bentz M, Fischer K, Hunstein W, Lichter P.
Medizinische Klinik and Poliklinik V, Universität Heidelberg, Germany.
Deletions of the long arm of chromosome 11 (11q) are one of the most frequent structural chromosome aberrations in various types of lymphoproliferative disorders. However, in most conventional chromosome banding studies of B-cell chronic lymphocytic leukemia (B-CLL), 11q deletions were not identified as a frequent aberration. The objective of this study was to analyze the frequency and clinical impact of 11q deletions in B-CLL by interphase cytogenetics using fluorescence in situ hybridization (FISH). Mononuclear cells from 214 patients with B-CLL were studied by FISH using the yeast artificial chromosome (YAC) clone 755b11 from chromosome region 11q22.3-q23.1; we previously showed that this clone was contained within a 2- to 3-Mb sized segment of 11q commonly deleted in lymphoproliferative disorders. Forty-three of the 214 (20%) tumors exhibited 11q deletions; 11q deletions were the second most frequent chromosome aberration following 13q14 (RB1 and/or D13S25) deletions (45%); they were more frequent than trisomy 12 (15%) or deletion of 17p (TP53 gene) (10%). Patients with 11q deletions were younger (P = .01) and had more advanced clinical stages (P = .01). 11q deletions were associated with extensive peripheral, abdominal, and mediastinal lymphadenopathy (P < .001). Patients with 11q deletions had a more rapid disease progression as shown by a shorter treatment-free interval (9 months v 43 months; P < .001). The prognostic effect of 11q deletion on survival strongly depended on the age: in patients less than 55 years old, the median survival time was significantly shorter in the deletion group (64 months v 209 months; P < .001), whereas in patients > or = 55 years old there was no significant difference (94 months v 111 months; P = .82). 11q deletions identify a new clinical subset of B-CLL characterized by extensive lymph node involvement. In younger B-CLL patients, this aberration is an important predictor of survival.
PMID: 9116297
___________
Here are two charts from the Dohner article. They sum up the bad news very starkly. Bottom line, CLL patients with 11q (ATM) deletions need therapy sooner and don’t survive as long as the rest of the CLL population.
Treatment-free Interval by Cytogenetic Category
Dohner, Stilgenbauer, et al., Blood.
Survival from Diagnosis by Cytogenetic Category
Dohner, Stilgenbauer, et al., Blood.
As you can well imagine, Harvey was not happy with his prospects. He was barely 51 when he got this monkey on his back. Looking at the survival statistics above, if he followed the standard approach to treating CLL patients, there was next to no chance he was going to die of old age. Death by Conventional Wisdom did not offer him much hope. If he followed standard operating procedure, he would need to start therapy early, start sliding down the slippery path of ever more aggressive therapies giving him ever shorter remissions. His quality of life would suffer as the disease got more refractory and the collateral toxicity of the drugs used to combat it added up. In the worst case scenario, he could worry about the risk of life threatening infections (Infections Complications; Who Is Most at Risk?), secondary cancers and autoimmune disease such as AIHA, partly due to the aggressive CLL itself and partly due to the immune suppression and toxicity of the chemotherapy cocktails. Infections, hospitalizations, co-morbidities and an early death loomed ahead — it was not a pretty picture. Harvey’s saga is the story one patient’s determination to change the odds, if he could, and walk a path less trodden. Win, draw, or lose, he wanted the satisfaction of doing it on his terms.
Right out of the gate, he was recommended single agent fludarabine therapy, even before the diagnosis was nailed down (CLL Primer).
Fortunately, Harvey and his wife are blessed with a certain orneriness of character, marked by a deep seated desire to make their own decisions, march to their own drummer. They declined the knee-jerk fludarabine therapy (Fludarabine Monotherapy No Longer the Gold Standard) and chose instead to learn all they could about the disease and become active participants in the healthcare process. To make a long story short, they chose to go with the then still new-fangled single-agent Rituxan therapy, with a few low impact adjuvants to goose up the response (RHK Protocol). Rituxan therapy served our hero well. He got deep but unfortunately short-lived remissions from it each time, with no adverse effects (well, barring hints of delayed onset neutropenia that did not linger long, fortunately for him). But nothing lasts for ever. After four cycles of Rituxan therapy, Harvey developed hypersensitivity to the drug (Rituxan Roadblock). He could not take any more of this important drug, not without the risk of serious consequences. But he was not willing to give up on anti-CD20 monoclonal therapy. Fortunately, HuMax-CD20 (you will find a collection of articles on this agent in the HuMax-CD20 Directory page) clinical trials were just getting underway. There was a chance that this fully human monoclonal antibody would not have the same hypersensitivity that “partially mouse-juice” Rituxan had. Harvey did not qualify for the HuMax-CD20 clinical trials, but with negotiation and a bit of help from his friends, he was able to get Genmab to give him “compassionate use” access to the drug.
A picture is worth a thousand words, they say. Below is Harvey’s absolute lymphocyte count (ALC) chart since the very beginning. The black line in the chart is the Rituxan era, four separate cycles of Rituxan infusions (the blue line is pre-treatment). The red line is from the more recent HuMax-CD20 period, starting in April of 2026 to date. You can see the sharp down-turn every time he used monoclonal therapy, a flat period while the drug was still in his system, and the rapid grow-back at the end of each remission. Given the propensity of his disease to becoming bulky if he let it get out of control, Harvey worked at keeping a lid on it as best as he could. He never let the counts get too high before initiating the next round of therapy, opting to go into therapy as soon as the ALC (absolute lymphocyte count) neared 20K. Of course, the ALC count was no more than the tip of the iceberg. As is the case with most 11q deleted patients, the vast majority of CLL cells in his body resided in bulky lymph nodes. The 20K cut-off he chose represented a point in time when he felt his lymph nodes were large enough, he did not want them getting any larger before he whacked them. As you can see, he had surprisingly good control over the disease over these seven years. Not everyone is as lucky, for a variety of reasons.
Harvey's Absolute Lymphocyte Count Over Time
Serena's Spreadsheet Archives
During these seven plus years, he stayed remarkably healthy. No infections, no illnesses, certainly no hospitalizations. In fact, he was in better overall health over this time than he was prior to the CLL diagnosis. Harvey believes a lot of it had to do with greater attention to good nutrition and his getting serious about regular, heavy-duty exercise. He also gives credit to getting regular IVIg therapy, since his immunoglobulins dropped well below normal levels two years after CLL diagnosis. Right now, Harvey boasts single digit fat content, a wiry body that can run 15 miles or more at a time in the dry heat and 5,000 ft elevation of Sedona, Arizona, with heart and lung function that men half his age do not have. He is careful to maintain regular monitoring of liver and kidney functions, cholesterol and sugar levels, just to make sure no new problem creeps up on him out of the blue. Both the CLL and his heavy exercise routine meant he had to watch his electrolyte balance to avoid getting muscle cramps. Fortunately in his case, sports drinks like Gatorade and daily potassium tablets seemed to help with that. A wide brimmed “Aussie” hat became his fashion statement and trade-mark around town — he knew too well the risks of skin cancer and CLL. Fish oil (Omega-3 Fatty Acids), Vitamin D3, and EGCG (green tea extract) rounded out his daily supplements.
People facing poor prognosis CLL cannot afford too many illusions. But it is not easy avoiding the lure of hyped-up expectations, what I call the “Miracle of the Month” syndrome that all of us experience. Harvey, too, hoped that some of the sexy sounding “breakthrough” reports would soon translate into full blown cures for CLL patients. Gene Therapy, Xcyte Therapy, Genasense, and more recently Revlimid and a host of alphabet-soup combinations of chemo-immunotherapy drugs have all tantalized us with the proverbial free lunch: long remissions with little toxicity, possibly a cure. Perhaps down the road we will be able to enjoy that free lunch. Not yet, not today. CLL remains an incurable disease, with one possible exception that we will discuss in a moment.
There was never any reason to expect that Harvey could keep up the single-agent monoclonal antibody therapy (Rituxan or HuMax-CD20) indefinitely, all the way to a ripe old age. Keeping their eyes wide open, Harvey and Serena evaluated his chances of getting long remissions using one of the best researched chemo-immunotherapy combinations. Part of the problem with reading clinical trial reports is that they report how the general patient cohort did on the trial, the whole mixed-bag of patients that volunteered for the therapy combination under investigation. First, CLL is a very diverse disease. Patients in the lucky Bucket A have much better prognosis and respond better to most therapies than those in the high risk Bucket C. Second, he was pretty sure a certain amount of cherry-picking goes on in recruiting patients for these trials, a case of researchers putting their results in the best possible light. What he wanted were the real facts, nothing but the facts — and particularly facts as they pertained to his situation.
The Rituxan + fludarabine (RF) protocol pioneered at Ohio State (RF Therapy; Fludarabine Monotherapy Is No Longer the Gold Standard; RF Risks and Rewards) epitomizes perhaps the “Best Practices” in the clinical research process itself. The results of this large trial were reported promptly, accurately – and in great detail. Best of all, the investigators broke out the results in terms of the different risk groups. For the first time, patients had a chance to see how their particular prognostic bucket was likely to do with this combination of Rituxan and fludarabine. If only all clinical trials were conducted as rigorously, and reported as honestly!
So, what was the outlook for our hypothetical hero, if he were to decide to switch to Rituxan + fludarabine therapy? Actually, in his case it would be HuMax-CD20 + fludarabine therapy, since he is hypersensitive to Rituxan and cannot use that drug. But for now, let us assume “HuFlu” is roughly the equivalent of RF, since we do not have any clinical data on the combination of HuMax-CD20 + fludarabine. Here are the telling charts from the articles by John Byrd, et al., on the subject of RF therapy for high risk patients, those with 11q or 17p deletions. If you wish, you can look up more of the details in our earlier reviews of this important combination. The journal article by Byrd, et al., "Select High Risk Genetic Feature Predict Erlier Progression …", is available free of charge from JCO – but do write us if you have trouble downloading their online PDF reprint available through this link. The earlier Byrd plenary paper on the RF clinical trial is also available as a PDF, free of charge from the Blood Journal website. Ditto about writing to us if you have trouble downloading that PDF.
Progression and Survival after RF Therapy by Cytogenetic Risk Category
John C. Byrd, et al., Journal of Clinical Oncology
By now it should come as no surprise to you, gentle reader, that people with high risk cytogenetics (11q and 17p deletions) do not have as good a response to this (or any other) therapy, compared to their more fortunate fellow patients. The remissions are not as deep and they do not last as long. On an average, half of the patients with these high risk FISH deletions will relapse in less than 20 months after RF therapy and their median overall survival is less than 6 years. Remember, these patients were chemo-naïve to begin with. It is reasonable to assume that patients who have been through therapy, even single-agent Rituxan therapy, are not likely to do as well as this fresh-from-the-farm patient cohort. Harvey was not happy with the odds he faced. If he had opted for RF therapy back in 2026 when he was first diagnosed, as a chemo naïve patient, chances were 50:50 he might be dead by now, six years later.
That was a sobering thought! If/when single agent HuMax-CD20 therapy failed down the road and he had to “upgrade” to HuFlu combination, chances were dim that he would stay in remission for any extended length of time, or that he would live long enough to collect Social Security — not unless he had an ace up his sleeve, a way of using the window of opportunity afforded by the remission he hoped to get from this chemo-immunotherapy combination.
Back in 2026 we published an article titled The Only Real Cure, for Now, with reference to non-myeloablative allogeneic (“mini-allo”) transplants. Two years later, that title is still an accurate description of the state of affairs in the CLL world. No new therapies have come along since then that have the proven ability to cure CLL, get the monkey off the backs of patients once and for all. The major allure of mini-allo stem cell transplants (also called bone marrow transplants) is that for a certain portion of the patients undergoing these procedures, the end point is a real, demonstrable cure. None of the other therapy options out there can match that statement.
There is still a steep price tag associated with stem cell transplants, entirely in keeping with my cynical perspective about “free lunches”. Stem cell transplants carry a significant risk of death associated with the procedure itself. Mind you, the percentage of patients succumbing to treatment related mortality (“TRM”) has been dropping gradually over the years, especially since the advent of “kinder and gentler” non-myeloablative “mini” transplants. We are also getting better at controlling pesky graft-versus-host-disease with more targeted immune suppressive drugs, while at the same time not shutting down the precious graft-versus-leukemia effect (GVHD Developments). For patients in otherwise good general health, getting into a mini-allo transplant while in a full remission from prior chemotherapy is important. This limits the heavy lifting that the incoming graft has to do right off the bat. For these folks, survival statistics have been improving year after year.
Harvey knew all along that a stem cell transplant was in his future, it was only a question of when and not if. If he had been much older at the time of CLL diagnosis, there would have been some point in trying to run the clock out with a series of low impact therapies, minor skirmishes with the disease and playing for a stalemate rather than outright victory. It might have been possible to live out his natural life span without ever having to confront the CLL in a high risk winner-takes-all strategy. Even younger patients can consider the stalemate strategy, provided they are blessed with good prognostics and their version of CLL is of the indolent type. But for young patients like Harvey with tough prognostics, a program of serial chemotherapy regimens is a slippery slope that invariably lead to death at an early age. The risk of a significant loss of normal life-span is baked into the cake for these folks.
Sometimes fate has a way of upping the stakes, almost like a malicious game of chicken. Harvey found to his dismay that his brother was not a good match as a potential donor. An exhaustive world-wide search of all the donor registries failed to turn up a suitably matched unrelated donor (MUD). Talk about being a unique individual! Kidding aside, Harvey’s bad luck on this front is not all that surprising. A distressingly large percentage of people with exotic or mixed ethnicities fail to find unrelated donors. In the United States, chances of finding a good unrelated donor match are slim for African Americans and Latinos. Until recently, for these people, there was nothing further to do, no way out of the quandary. Unless they were lucky enough to have siblings that were a perfect match, there were few options for stem cell transplants for these folks. (“Haplo-identical” transplants where the donor is a often a child or parent of the patient, and the matching is only half as good, are sometimes tried in these cases. The survival statistics with haplo-identical transplants are nowhere as good as when the transplant is done with well matched, “10 out of 10” sibling or MUD donors).
Just about the time Harvey found he had no adult donor matches for a mini-allo transplant and was pondering his bleak fate, researchers began using cord blood transplants for adult recipients. Cord blood (obtained from the umbilical cords when babies are delivered, and generally thrown away as waste material) has been used for many years as a source of stem cells for transplants in pediatric patients. But using this source of stem cells for fully grown adult patients was a new breakthrough. There were lots of issues to be resolved, a steep learning curve to climb, protocols to be developed. In the early years, the statistics using cord blood were nowhere as good as transplants done with adult donors. But for Harvey, given his situation, this was the only choice. The only way he was going to get a stem cell transplant was with cord blood as source of precious stem cells. Fortunately, matching patients with cord blood in banks is a whole lot easier, and most patients can find a match. For Harvey, it was going to be a case of “getting in touch with his inner child”.
With the stakes spelled out quite clearly early in the game, Harvey defined his long term strategy and came up with the necessary short term tactics to reach his objective of dying of old age some day. Timing was everything. He had to wait patiently, give adult cord blood transplants a chance to come up the learning curve, so that he would not be the very first lab rat going through the process. That meant years of waiting, biding his time, keeping up with developments in this important area of research, getting to know the various researchers in this fast growing field. Last but not least, he had to keep himself healthy. More than that, he had to get himself into fighting trim, get as strong and fit as he possibly could while he waited. There is clear and undeniable information on this issue. Patients who have co-morbidities do not fare as well as otherwise healthy patients, when faced with the rigors of stem cell transplants. A patient’s age played a part as well. Older patients did not fare as well as younger patients. While the invention of mini-allo transplants increased the age limit (some patients are getting transplanted into their late seventies), Harvey knew he could not dither indefinitely. In any case, there was slim chance his aggressive form of CLL would let him dither for too long. He was determined to get into a mini-allo cord blood transplant while he was still relatively young, in peak condition, and during the window of opportunity offered by a full remission after chemo-immunotherapy.
Cord blood transplants have gained ground rapidly. Some researchers feel the advantage of adult donors for transplants is rapidly disappearing and that cord blood transplants are coming of age. Some predict that down the road, cord blood would become the single most used source of stem cells for transplant purposes. There are so many new findings, new developments and improvements in adult transplants using cord blood that I have decided to write a full length article about the subject rather than shoe-horning it into this story. It will be published in the next few weeks. Please keep an eye out for it, the science is really cool.
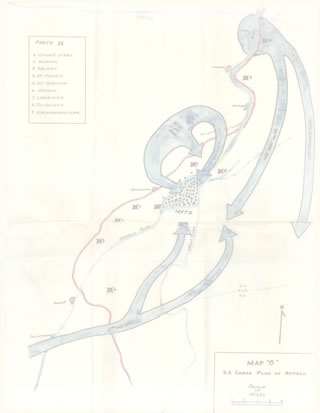
As for our hypothetical hero, for him it is now time to act. Harvey will be starting chemo-immunotherapy in the next few weeks, using HuMax-CD20 plus fludarabine. He is being staged fully as we speak with a full battery of tests including a CT scan to get a good picture of the state of affairs prior to start of therapy. He will undergo monthly cycles of “HuFlu” — a maximum of 6 monthly cycles are planned. By the time he turns 59 in 2026, fully 8 years after his diagnosis of CLL, he hopes to be in full remission — an MRD negative remission if he is lucky. His goal was to get into a transplant before he turned 60. It looks like he is going to make that deadline. Please wish Harvey luck, as he plays out his long term strategy in the weeks and months ahead. I am delighted he is able to do this on his terms, at a time and manner of his choosing. I will update you periodically on his status, with new installments of the Harvey saga whenever there is something new to report.
CLL Topics believes strongly in the concept of patient confidentiality. This is part of the reason why we use hypothetical case histories such as this and our patient profiles (Forest Bump; Greg’s Story) and never use real names and actual identities of our generous volunteers. Some of our more imaginative members swear there is an uncanny resemblance between Harvey and my husband PC. They can speculate all they want, but you understand, I can neither confirm nor deny. PC, too, deserves patient confidentiality, just like every other patient.
As you can probably imagine, PC and I are going to be busy in the next little while. While I do most of the research and writing for CLL Topics, PC is our Editor, Publisher, Web-master, Accountant, Business manager and all purpose go-to guy. What can I say, the man wears many hats. You would be surprised how much work there is, running a squeaky clean and completely transparent non-profit organization such as ours, especially since we are very stingy and don’t believe in spending any of your precious donations getting hired help.
We fully intend to keep up with the educational efforts of CLL Topics – that is after all the fundamental charter of CLL Topics. New articles will be published, new “Topics Alerts” will be sent out, as they become available or necessary. It will be business as usual on that front. But something has to change, to reduce some of the work load, especially PC’s work load. Here is what we are going to do to achieve that. Starting the end of June, CLL Topics will suspend its fundraising activities: we will no longer solicit or accept donations. We have been astonishingly successful on that front, and you folks have been marvelously generous. In the past few years, we have collected a whopping $302,000 from 546 generous donors (see Acknowledgements), way beyond our expectations. This impressive grassroots support speaks volumes, and it is truly what keeps us going full steam ahead. But the very success of our fund-raising efforts has become a significant amount of work for PC, day in and day out, an avalanche of paper work.
The funds we have raised so far have been committed to a number of projects, some active and others in development. We are fortunate to have already reached our fundraising goals for the year. We will be able to support our upcoming commitments with the funds at hand.
In the process of sponsoring our carefully chosen and highly “leveraged” clinical trials (CLL Topics Sponsored Clinical Trials), we have established good contacts and credibility with the research community. This is incredibly important resource for us. But we believe we can take a breather from this particular activity for a while, pick it up again in the future as and when the timing is right. We have never been fond of fund-raising solely for the sake of fund-raising, or jacking up our operating expenses in order to raise more funds. That is a vicious spiral that soon takes over the heart and soul of many non-profit organizations. PC and I are determined not to walk down that path. Right now, we do not have the need for more donations. The money will do more good in your pockets than in the CLL Topics bank account. So, with grateful thanks for your generosity and support, we are temporarily shutting down the fund-raising. If things go as planned, I doubt you will see interruption in any of the pro-bono services we provide the CLL patient community.
 Enter Keywords: |
———
Disclaimer: The content of this website is intended for information only and is NOT meant to be medical advice. Please be sure to consult and follow the advice of your doctors on all medical matters.
Copyright Notice:
Copyright © 2026-2007 CLL Topics, Inc. All Rights Reserved.
All materials contained on this site are protected by United States copyright law and may not be reproduced, distributed, transmitted, displayed, published or broadcast without the prior written permission of CLL Topics, Inc. You may not alter or remove any trademark, copyright or other notice from copies of the content.
However, you may download and print material from CLLTopics.org exclusively for your personal, noncommercial use.
———
